If you’re getting ready to deploy to a high-altitude environment such as the mountains of Afghanistan, you might experience altitude sickness when you first get on the ground. Prevention is important, so you’ll want to prepare in advance. Since it’s a little harder to breathe, it might seem like using your gas mask or high-altitude training mask during exercise will help, but it turns out they don’t work too well for altitude acclimatization.
Increasing the strength of your diaphragm and the muscles between your ribs—the respiratory muscles that help you breathe—will improve aerobic fitness, especially for long-duration tasks. However, using your military gas mask or other commercial mask device as a method of respiratory muscle training (RMT) isn’t going to prepare you for higher elevations. It was made to protect your lungs, eyes, and face from chemical and biological agents, radioactive particles, and battlefield contaminants. And it doesn’t create enough airflow resistance to help improve aerobic capacity. In addition, it wasn’t designed as exercise equipment. Similarly, commercially available high-altitude training masks, or normobaric hypoxic devices, provide little benefit to acclimatize you to training in a low-oxygen environment. Read more in the U.S. Army Research Institute of Environmental Medicine’s (USARIEM) information paper on gas masks and commercial products and HPRC’s summary on normobaric hypoxic devices for exercise training.
Training for high-altitude environments is very difficult outside of a laboratory environment, unless you’re able to gradually train yourself at altitudes over 5,000 ft. This type of training typically requires either a hypobaric chamber, which reduces the air pressure and oxygen levels to simulate altitude, or very precise forms of RMT such as voluntary isocapnic hyperpnea training (VIHT). VIHT requires you to maintain high breathing rates for upwards of 30 minutes at a time and a close regulation of oxygen and carbon dioxide gas exchange.
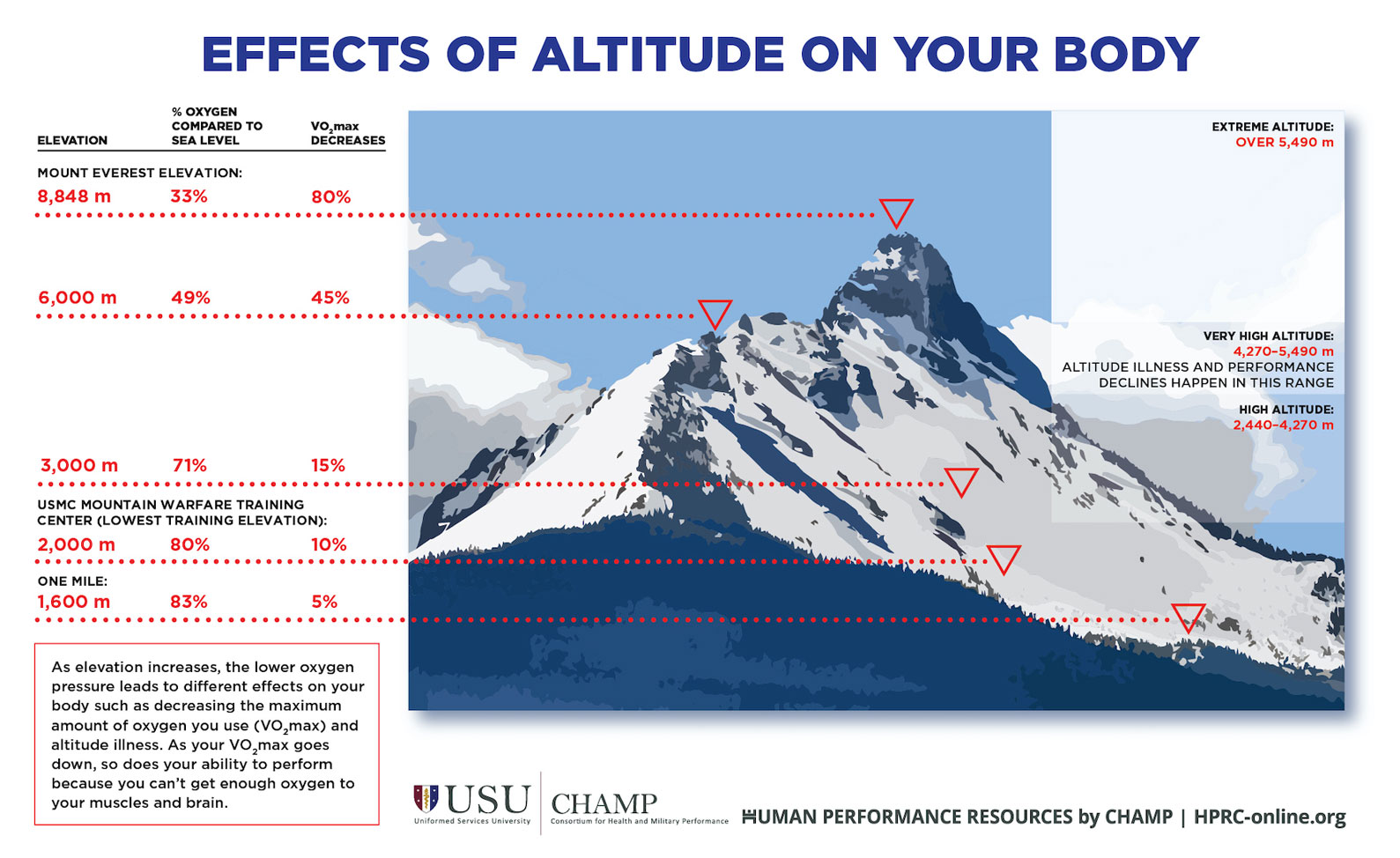
There’s no readily accessible and practical method to train for altitude without either actually exposing yourself to high-altitude or expensive laboratory equipment. So, when you’re getting ready to deploy to a mountain environment, go TDY to mountain training, or PCS to Denver, it’s essential to maintain high levels of physical fitness to make the transition easier on your body and prevent altitude sickness.