Your body has 206 bones, about 600 muscles, and 360 joints. If you understand how the bones connect and create joints and get moved by muscles, it can help optimize your workouts, prevent injuries, and help you work around injuries when they do happen. In this article, you will read about the different structures of the body, what they do, and some names of related injuries. This article will also cover the basics of tissue healing, which explains why it can take so long to fully recover.
Bones
Bones provide the framework for the human body. During childhood, your bones grow from growth plates and get longer, thicker, and denser. Your bones continue to grow through childhood, building about 90% of your bone mass (by 18 for women and 20 for men), and your last growth plate closes by about age 25. After that, the bone will not get bigger or add mass, but it will maintain and eventually start to lose mass as you age. You build bone mass and replace damaged bone by using vitamin D to absorb calcium from food. This is why it is especially important for children and adolescents to have enough vitamin D and calcium in their diets. In fact, osteoporosis is said to be a childhood disease that presents in adulthood. As you age, your bone mass and bone strength will decrease—even faster as you get older—so it’s important to maximize peak bone mass during adolescence.
A few different kinds of bone injuries can happen. The most severe is a fracture, where your bone breaks after a traumatic event, such as a fall. The different kinds of bone fracture—crushed, splintered, a clean break, etc.—can indicate how well it will heal on its own or if it will need surgery. Other common terms for a traumatic fracture are “open fracture” and “compound fracture.” Both refer to an open skin wound near the fracture site. Open fractures, with or without the bone exposed, are serious injuries because they bring a big risk of infection.
Other types of bone injuries are stress fractures and bone-stress reactions. A stress reaction is an overuse injury that happens when high loads are put on a bone over a period of time without enough time to recover. One example is when you increase your running volume too quickly without enough recovery days. If a stress reaction isn’t caught and treated early, it can turn into a stress fracture, where the bone actually breaks. Endurance athletes and physically active people—especially those with relative energy deficiency in sports (RED-S) or the Female Athlete Triad—are particularly at risk for developing stress fractures.
 Joints and ligaments
Joints and ligaments
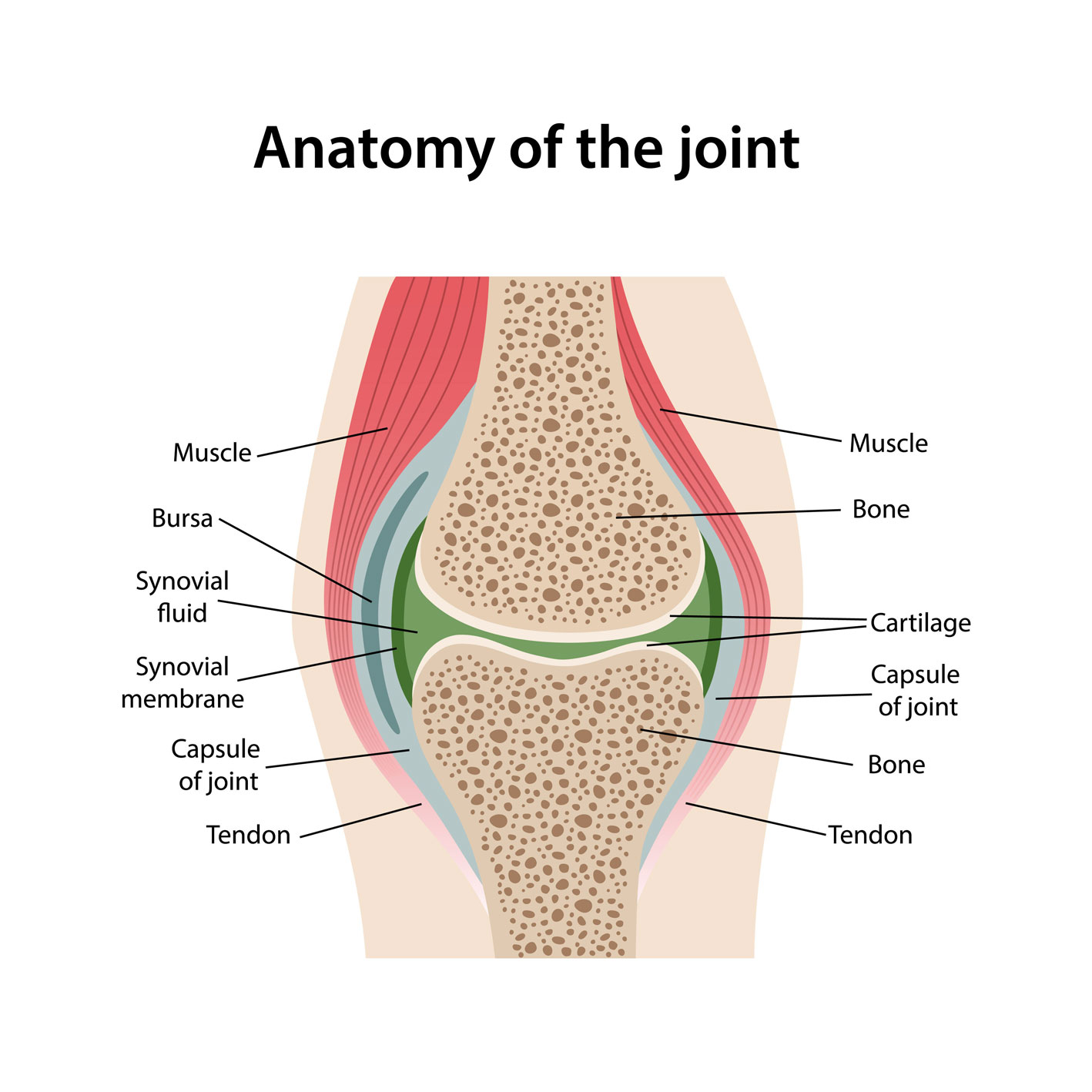
A joint is where two or more bones connect. Your body has 3 types of joints. Fibrous joints exist where the bones are fused and don’t move, such as the different bones in your skull. Cartilaginous joints are where the bones are connected by a type of cartilage and move a little bit, such as the vertebrae in your spine connected by intervertebral disks. Synovial joints make up the major joints in your shoulders, elbows, hips, knees, and ankles. In these, the joint is surrounded by a capsule filled with synovial fluid, which lubricates the joint and provides nutrients to the area.
The bones in the cartilaginous and synovial joints are connected by fibrous structures called ligaments, which are designed to limit motion in the joint. Injuries to ligaments are called sprains. These injuries can range in severity, including an overstretch—where the ligament is stretched too far—a partial tear, and a full tear. When someone says, “It’s just a sprain,” it could mean anything from a mild injury to a severe full tear.
Muscles
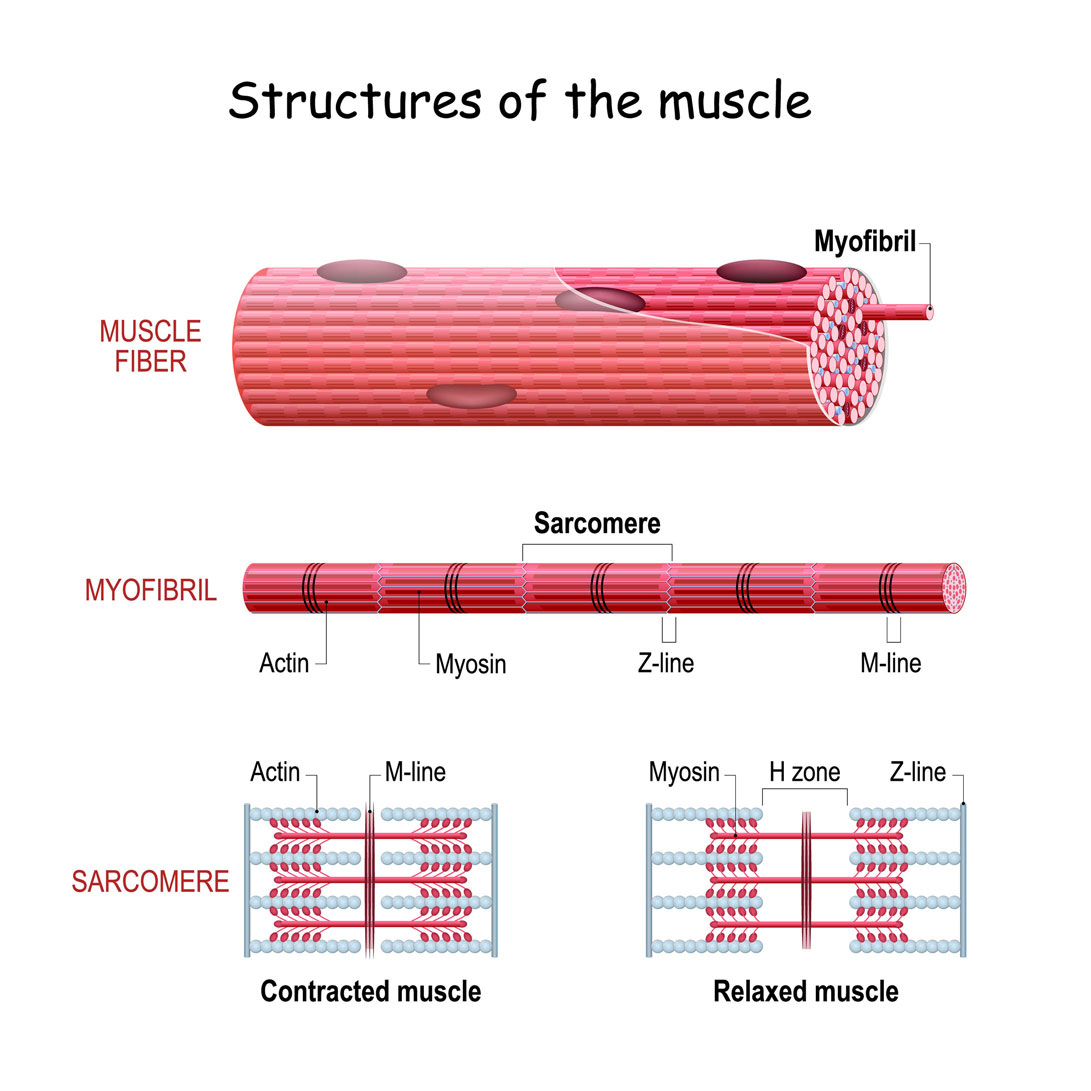
You have 3 different types of muscle fibers in your body that contract to move your bones. Type I fibers—also called slow-twitch fibers—produce the least amount of force but are most resistant to fatigue. They draw most of their energy from your aerobic energy system and require oxygen to breakdown carbohydrates and fats for energy. These muscular endurance fibers are used to maintain posture and for long bouts of endurance exercise.
Type II fibers—fast-twitch fibers—have two sub-types. Type IIA fibers produce a medium amount of force somewhat quickly, and Type IIX fibers produce a large amount of force very quickly. Type IIA uses energy from a combination of aerobic and anaerobic sources. Type IIX fibers draw energy from anaerobic sources. Anaerobic energy production does not require oxygen and happens faster than aerobic energy production. This allows you to produce high levels of force very quickly. The tradeoff for speed and force means anaerobic energy sources will tire faster.
 All muscles have both fiber types, regardless of your DNA. However, the number of fibers of each type varies and is dictated by your genetics. People who are successful marathon runners have mostly Type I muscle fibers, compared to sprinters, who mostly have Type II. Type II subtypes can change with training. Over time, high-volume, moderate- to high-intensity training that uses your aerobic energy system can cause Type IIX muscle fibers to convert to Type IIA fiber types. If you stop training to stress your aerobic system, the Type IIA will convert back to Type IIX. If you train at high intensity with low volumes, such as sprinting or muscular strength training, Type IIA can convert to Type IIX. It’s unclear if you can convert between Type I and Type II fiber types.
All muscles have both fiber types, regardless of your DNA. However, the number of fibers of each type varies and is dictated by your genetics. People who are successful marathon runners have mostly Type I muscle fibers, compared to sprinters, who mostly have Type II. Type II subtypes can change with training. Over time, high-volume, moderate- to high-intensity training that uses your aerobic energy system can cause Type IIX muscle fibers to convert to Type IIA fiber types. If you stop training to stress your aerobic system, the Type IIA will convert back to Type IIX. If you train at high intensity with low volumes, such as sprinting or muscular strength training, Type IIA can convert to Type IIX. It’s unclear if you can convert between Type I and Type II fiber types.
A simple way to describe a muscle contraction is to imagine you are pulling an object towards you hand-over-hand with a rope. As the muscle contracts, you pull with your left hand, then your right. When the muscle relaxes, it is as if the object gets pulled away from you, and you slowly let the rope go without it sliding through your hands.
Injuries to muscles are called muscle strains, and they are graded based on the severity. Using the rope analogy, a strain happens when the object is pulled away from you with too much force. The rope can stretch, fray near the middle, or break completely.
Tendons
Tendons connect muscles to bones and transfer the force from the muscle to move the joints. Tendon injuries are called “tendinopathies,” or previously known as tendinitis. Tendinopathies happen when the tendon breaks down from overuse, repetitive activity, or age. If the injury becomes severe, it can lead to a tendon rupture. Tendons can also tear off the bone or away from the muscle.
Cartilage
Your body has 3 different types of cartilage, a type of connective tissue whose purpose varies by type. Elastic cartilage makes up your outer ears. Fibrocartilage is more rigid to provide support. The meniscus in your knee is made of soft fibrocartilage, and it’s designed to provide a better surface for your femur (thigh bone) to connect to your tibia (shin bone). Without a meniscus, the round bottom of the femur needs to sit on the flat top of your tibia, which is not very stable. The meniscus creates a shallow socket for the femur and provides some shock absorption when you walk. Hyaline cartilage is smooth, makes up most of the cartilage in your body, and is designed to help reduce friction in your joints.
The most common cartilage injury is osteoarthritis (OA). OA can happen after an injury, such as an ACL sprain, or through overuse. Other types of cartilage injuries include chondromalacia—a softening of the cartilage—and osteochondritis dissecans (OCD). OCD occurs when a small piece of cartilage and bone separates from the rest of a bone. Depending on the size of the OCD, it either needs to be surgically removed or placed back into position with a pin or screw.
Cartilage injuries can be difficult to recover from because cartilage receives little- to no-blood supply. Nutrients and repair cells aren’t able to easily get to the area to heal the damage without a good blood supply. When an injury is severe, surgeries can be performed to help repair the damage or remove the unhealed, damaged tissue.
Nerves
Bones, muscles, ligaments, and tendons all have nerve fibers. The nerves are responsible for sending signals about the health of the tissue, information about the position of a joint, muscle activation, and other functions. When you sustain an injury, the nerve fibers can be damaged and affect how those signals are sent. For example, when you sprain your ankle, the nerves in the ligaments and joint capsule are stretched and damaged. This leads you to lose proprioception—your sense of how your ankle’s position relative to your body and the ground—and explains why your balance is affected.
Tissue healing
After an injury, your body starts the repair process almost immediately. The first step in the healing process is the inflammation phase. Your body sends different chemicals and cells to clean the area and remove damaged tissue, making it red, hot, swollen, and tender. The inflammation phase usually lasts 2–4 days. If it doesn’t happen, there is no signal to repair the damaged tissue. Experts recommend that you don’t take anti-inflammatory medicines, such as ibuprofen (Advil and Motrin) for a few days after the injury. You want your body to heal naturally. Inflammation becomes a problem when it isn’t initially effective, so the chemicals and cells stick around longer than they should. This leads to prolonged pain, swelling, and loss of function. You can end up with damage to healthy tissue. Injuries are often immobilized with splints, walking boots, crutches, or other devices during the inflammation phase.
The repair phase starts around day 4 and lasts about 4–6 weeks. In this phase, a scar forms over the damaged tissue. The scar is weak and needs to be allowed to build up before you stress the tissue heavily again. In a normal healing process, very little “scar tissue” —excessive scarring—is formed. If the inflammation phase lasts too long, it extends the repair phase, which can lead to scar-tissue development. During the 6 weeks when repair takes place, the injured tissue is progressively loaded by exercising the area, which helps strengthen the repair. The progressive loading is essential for the injury to heal properly, and for you to return to full duty as fast as possible. After 6–8 weeks, many injuries are healed enough that you can feel close to 100%. But without the progression leading up to that, you won’t be healed enough to work or play sports without risking re-injury.
The remodeling phase (which overlaps with the repair phase) starts around week 4. This long-term process—where the scar created during the repair phase slowly converts into normal tissue—takes up to 2–3 years to complete.
The length of each phase depends on several factors—the severity of the injury, how much the area swells, how much the injury bleeds, etc. When you work with a medical provider to rehab an injury, they use your pain as the guide to progress your exercises. You shouldn’t feel pain—with a few exceptions—during this time. If you start to feel pain, you might be progressing too fast.
When injuries aren’t treated—or are not properly and progressively loaded—you can run into long-term issues. After an ACL surgery, it’s important to bend your knee a day or 2 after surgery, and then bend it further every day. This adds a light stretch to the new ACL and prevents scar tissue from forming. If scar tissue builds up, you can lose range of motion and need another surgery to remove the excess. Progressive exercise of the injury helps repair the damaged nerves. This helps you regain proprioception and relearn how to fire the muscles that move the joint. This will help prevent you from reinjuring the same body part.
Bottom line
Understanding basic anatomy will help you improve your military fitness. It gives you a better idea of how your musculoskeletal system works, gets injured, and heals. Future articles will introduce different muscle groups and discuss how they work together to perform common exercises and military-specific tasks.
