Diabetes mellitus (diabetes) is a group of metabolic disorders that affects how you use blood sugar. When you exercise, your body uses blood sugar to make energy. If you have diabetes, it’s critical to pay careful attention to your blood sugar levels before, during, and after exercise so you don’t have a diabetic emergency caused by low blood sugar.
What’s diabetes mellitus?
The two main types of diabetes are Type 1 and Type 2. Type 1 (T1DM), previously called juvenile diabetes, is an autoimmune disorder where your immune system destroys the cells in your pancreas that make insulin. Type 1 diabetics aren’t able to produce insulin, so their muscles can’t use blood sugar without it being injected. Type 1 diabetes is usually caused by genetics. Type 2 diabetes (T2DM) happens when your muscle and fat tissues are less able to use the insulin that you do produce, making you insulin resistant. The most common causes of type 2 diabetes are obesity and inactivity that decrease insulin production and sensitivity.
Glucose—a type of sugar—is required for energy production in cells. When your blood sugar gets too low (hypoglycemia), your cells won’t have enough energy, and you can experience heart palpitations, dizziness, sweating, and shakiness. In severe cases, you might be at risk for muscle weakness, fatigue, seizures, and loss of consciousness. High blood sugar (hyperglycemia) can cause dehydration, increased thirst, and muscle weakness. In severe cases, it can cause nausea and vomiting, abdominal pain, and diabetic coma. Chronically high blood sugar (measured by your A1c blood test) can damage your nerves, arteries, eyes, and kidneys over time as well.
Insulin controls blood sugar
Blood sugar is controlled by tissues in the pancreas that sense high levels of glucose and send insulin into your bloodstream to encourage muscle and fat tissues to absorb it. That lowers your blood sugar and brings it towards the “normal” range. When your blood sugar gets low, or you experience stress (physical, mental, or emotional), your pancreas releases a hormone (glucagon) to tell your fat cells to release fatty acids and your liver to make glucose. This raises your blood sugar.
Regular exercise is a powerful way to control your blood sugar, lose weight, and improve your health span, but it only works if you can be consistent. Even low-intensity walking will have a meaningful impact on blood sugar control if you do it regularly.
What happens during exercise?
Your body experiences exercise as stress, which can vary based on the type of exercise you’re doing. Longer bouts of low-to-moderate intensity exercises cause your body to respond differently than shorter bouts of high-intensity exercise.
Muscle tissue can use over 10 times more energy when you exercise than at rest. To fuel these energy demands, muscle tissues are signaled by insulin to absorb blood glucose. Exercising muscle cells become more sensitive to insulin when you exercise so that it’s easier for them to sense it in your bloodstream. Muscles can keep this higher insulin sensitivity for up to four days after the exercise session. Regular exercise also improves long-term blood sugar control by increasing mitochondrial density (the number of mitochondria in your cells), muscular strength, size, and endurance.
During exercise with a long duration, stored fat breaks down into individual fatty acids and enters your bloodstream. That fatty acid travels to the liver and gets turned into glucose before traveling to the exercising muscle for use as energy. A relatively small amount of free fatty acids travels straight to muscle cells for direct fuel use.
When you exercise, your “fight-or-flight” (sympathetic) nervous system turns on and tells your pancreas to release glucagon and raise blood sugar. At the same time, your pancreas senses a fall in blood sugar from it being used by your muscles. This fall in blood sugar stops the release of insulin. Even though you’re producing less insulin during exercise, the rise in insulin sensitivity of your muscles is enough to use the little bit that’s still in your blood.
All of this is what happens when you exercise—how much it happens depends on the type of exercise you’re doing. At low intensity, such as walking, your muscles are using glucose, but your liver and fat can easily keep up. You probably aren’t at risk of hypoglycemia or hyperglycemia. At moderate intensities such as fast walking or jogging, your muscles have a greater glucose demand, and it’s hard for your liver and fat to keep up. This can result in hypoglycemia, especially after 30–60 minutes. During short, repetitive bouts of high-intensity exercise, your muscles use their energy (adenosine triphosphate [ATP]) and creatine phosphate stores. You start burning glucose quickly, but it takes a minute or two to build your ATP and creatine phosphate stores back up. You also experience such a strong stress response that your glucose production can outpace muscular absorption. This can cause brief hyperglycemia, especially in people with T1DM. Brief hyperglycemia is a normal, healthy response to stimulus and is usually only dangerous and the very extremes—for example, if your blood sugar is higher than 250 mg/dL and there are ketones present in your blood. You might start to feel some symptoms of hyperglycemia and not feel well. Resting for a few minutes and doing some low-intensity, active-recovery exercises will help your body use some of the excess blood sugar.
I’m diabetic. How should I exercise?
In general, those with diabetes should follow the recommendations for exercise in the Physical Activity Guidelines for Americans: 150 minutes of moderate-intensity (or 75 minutes of vigorous-intensity) activity in addition to two sessions of resistance training per week.
If you have T1DM, pay close attention to your blood sugar, especially if you’re doing longer duration, low- or moderate-intensity exercise. Remember, low- and moderate-intensity exercise will cause your blood sugar levels to fall. Hypoglycemia can lead to severe injuries or death if you don’t monitor your levels and adjust your insulin and carbohydrate intake accordingly.
If you have T2DM, blood sugar monitoring requires a little less attention. T2DM causes high blood sugar levels, and it’s very unlikely that they fall to a dangerous level. For high-intensity exercise, even though it can lead to brief hyperglycemia during the workout, your sugar levels will start to come down during your rest periods and immediately after the workout. High-intensity exercise is also very effective for controlling blood sugar levels over the long term as your muscles become more sensitive to insulin. If you’re currently on insulin, whether you have T1DM or T2DM, you need to monitor your sugar levels closely before, during, and after exercise.
Even if you don’t meet the guidelines, any activity is better than no activity, and the benefits almost always outweigh the risks (when you exercise safely). Even low-intensity walking will have a meaningful impact on blood sugar control if you do it regularly. Find an exercise routine that you can comfortably and safely perform and stick to it!
If you’re new to regular exercise, start slow and remember that anything you do is worthwhile. Start with short walks or bike rides and build them into your weekly routine. Once you work it into a habit, add more. Make your walks longer, or add another day. Keep your bike rides the same, but add a jog on another day. Try resistance training or swimming, if you never have. Whatever you choose, make sure that you only progress to the “next step” when you’re comfortable with what you’re doing. Regular exercise is a powerful way to lose weight, control your blood sugar, and improve your health span, but it only works if you can be consistent. It’s better to be consistent going for an evening walk three times per week than it is to run hard every day for two weeks only to burn out and do nothing for a month afterwards. Lastly, as you progress your exercise in duration, intensity, or frequency, make sure you know how to manage your blood sugar consistently with your current routine. This will give you a great foundation as you move on to your next challenge.
Fueling considerations during exercise
When a type 1 diabetic begins an exercise session, their insulin level is already established by what they have injected with an insulin pump or syringe, and will continue to act on their tissues. Type 1 diabetics are at risk for severe hypoglycemia during exercise. Hypoglycemia can be prevented or quickly corrected by adjusting bolus insulin, basal insulin, or carbohydrate intake before and during exercise.
Since insulin levels will rise and fall normally for people with T2DM, fueling to maintain blood sugar levels is less of a concern. People with T2DM have insulin: They’re just less able to respond to it. Experts generally recommend exercising within 90 minutes of a meal to help prevent your blood sugar from spiking too much after eating.
Just like everything else for T1DM, regulating blood sugar during exercise revolves around careful trial and error, and finding what works for you. Add exercise to your blood sugar logbook. Record your blood sugar 30–60 minutes before exercise, what exercise you performed, how it felt, and your blood sugar after. As always, communicate with your medical provider or diabetes educator who helps manage your diabetes. They should be able to help you interpret blood sugar swings.
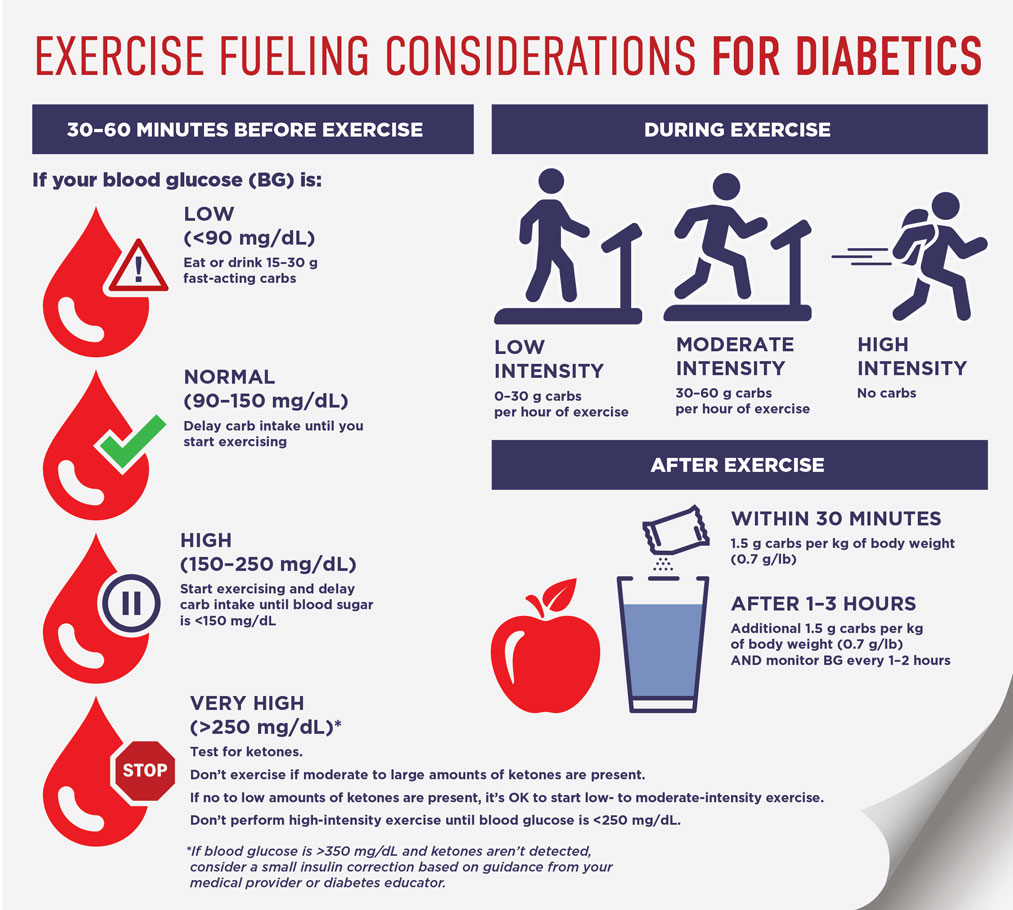
Here are some tips to help find a blood sugar maintenance plan that works for you when you exercise. The chart below also contains general guidelines. It’s also important to work out your own specific timing and amounts with your medical provider or diabetes educator.
Before exercise. 30–60 minutes before you exercise, consider your current blood glucose level and the intensity and duration of your upcoming session. If you plan to exercise within 90 minutes of bolus insulin administration, consider decreasing that dose.
During exercise. As you exercise, make sure you hydrate and continue to consume high-glycemic foods to maintain your blood sugar. These are foods like fruit juice, pretzels, rice, honey, and most candies. Trial and error is the most reliable way to find foods or sport supplements that work for you and also don’t cause stomach discomfort or nausea during exercise. Talk to your doctor about decreasing your basal insulin in preparation for especially long and difficult workouts, like if you’re training for a half- or full marathon.
For some T1DM athletes who are exceptionally fit, 60 g of carbs per hour might still not be enough to maintain blood glucose. For these athletes, consumption can be increased to up to 90–100 g per hour using a glucose:fructose ratio of 2:1 when advised by their medical provider. One of the biggest mistakes athletes make is restricting carbs to control blood glucose, which can end up compromising performance and isn't always necessary. For optimal performance, these athletes should consult with a Registered Dietitian or Certified Diabetes Educator to develop a tailored fueling plan.
After exercise. If you finish exercising and are hypoglycemic, or have finished a session longer than 90–120 minutes, it’s important to consume enough carbs to replenish glycogen and maintain blood glucose. For most exercise bouts, if you have fueled appropriately before and during, you shouldn’t need much to recover afterwards.
Bottom line
Exercise is a powerful tool for people with diabetes to control their blood sugar, lose weight, and generally be healthier. Diabetic individuals should carefully consider how exercise affects their bodies and will strongly benefit from making exercise part of their weekly routine.
