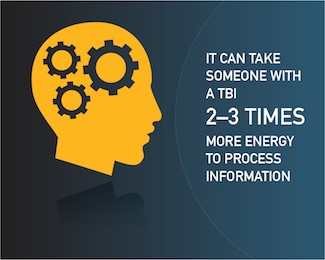
 What’s 2 × 2 equal? How about 4 × 4? The speed at which your brain processes those questions and the energy it takes you to decide on an answer is likely to be minimal—unless you have a traumatic brain injury (TBI). For Warfighters diagnosed with TBI, making decisions and remembering things can lead to fatigue that spills over into your family. Still, it’s important for loved ones to try to be patient and understand that Service Members with TBI might take longer to answer questions about what day it is or even where they put their wallet. There are many ways to help your Warfighter cope with TBI symptoms at home too.
What’s 2 × 2 equal? How about 4 × 4? The speed at which your brain processes those questions and the energy it takes you to decide on an answer is likely to be minimal—unless you have a traumatic brain injury (TBI). For Warfighters diagnosed with TBI, making decisions and remembering things can lead to fatigue that spills over into your family. Still, it’s important for loved ones to try to be patient and understand that Service Members with TBI might take longer to answer questions about what day it is or even where they put their wallet. There are many ways to help your Warfighter cope with TBI symptoms at home too.
Family members often become the main source of caregiving support for those recovering from TBI. Your Service Member might have trouble concentrating, memory loss, sensitivity to light or noise, sleep problems, or mood swings. TBI also can impact your loved one’s senses of taste and smell, appetite, sex drive, and balance. Brain processes that were once automatic are now slower or missing and need to be rebuilt as well.
How can families support their Service Members with TBI?
Recovery from a TBI can go smoother when family members provide care and emotional support to help manage their Warfighter’s TBI symptoms. For instance, they might need to talk slower, repeat themselves, and wait longer for responses. It’s also important to know that memory loss that comes with a TBI means your loved one might not recall important family events and other moments.
Keep in mind learning to adapt to your warrior’s needs helps foster family resilience. Making some changes around your home and to your family’s routines can help reduce everyone’s stress too. Try the following tips to help your Service Member cope with TBI symptoms.
Memory loss
- Create morning, afternoon, and evening checklists that include simple tasks they can do without much effort. Include things such as “check to see the coffee pot is turned off,” “take your medicine,” “lock the front door,” or “make sure the stove is turned off.”
- Write out weekly events—including chores and due dates—on a whiteboard. Use a system to mark who’s doing what and which ones are done.
- Encourage your Service Member to use a phone or tablet to record conversations, make pop-up reminders, or type out notes after a conversation to help recall things later.
- Help your Warfighter use the calendar on his or her mobile device to track appointments and store phone numbers.
- To help with writing down reminders, leave notepads and sticky notes all over your house. And store all written reminders in one place, so you can track what needs to be done.
- Choose appliances that automatically shut off.
- If you have kids, play memory games together to improve everyone’s skills.
Sleep problems and fatigue
- Stick to a regular sleep schedule as much as possible.
- Practice good sleep hygiene. Sleep in comfortable clothes and adjust the room temperature to be a bit colder than what’s typical (60–67°F).
- Visit your healthcare provider to help assess and treat sleep apnea if it impedes sleep quality.
- Make sure you plan enough downtime in between daily, weekly, and monthly scheduled events.
- Plan recovery time after big events.
Vision problems and sensitivities to smells, sounds, and tastes
- Install smoke alarms with voice commands in your home if your Service Member is experiencing problems with their sense of smell.
- Set up an area in your home that’s low stimulation with adjustable lighting and simple decor.
- Help your family choose the maximum volume for the TV when everyone is home.
- Set quiet hours in your home, where everyone agrees to turn off the TV, keep voices low, and use earbuds or headphones while listening to music.
- Decide which herbs and spices are suitable for family meals, especially if your Warfighter is sensitive to certain smells or tastes.
- Discuss any swallowing concerns to help identify which foods are easier or harder for your warrior to swallow.
- Listen to audio books or podcasts together or read books with large print.
Learn more
Lastly, find out what recovery after a TBI looks like. Understanding typical changes in the behavior, mood, and personality of someone who has experienced a TBI can help. It’s still possible to build strong relationships after a TBI, but it just might look different than you initially planned.
